‘Huge day’: Voluntary assisted dying launches in SA
South Australia’s landmark voluntary assisted dying laws come into force today, with one terminally-ill advocate welcoming it as a “weight off his shoulders”.

Voluntary assisted dying advocate Kym Watson says he feels "proud" that the legislation is now in force. Photo: Stephanie Richards/InDaily
The implementation of the Voluntary Assisted Dying (VAD) Act follows decades of advocacy, with those in support arguing the laws will offer people a safe and dignified way to end their life.
For 66-year-old Kym Watson, who has multiple systems atrophy, the implementation marks a “huge” moment in his life.
“Today, I am so proud to be a South Australian,” the Goolwa grandfather told reporters this morning.
“Empathy and good will has surfaced to such a degree that people with terminal illnesses can have the opportunity to pass in peace and be with the people they love.
“I can’t say how grateful I am for… this happening.”
Watson described multiple systems atrophy as “the ugly side of Parkinson’s (Disease), which shuts things down inside of you”.
He said having the neurodegenerative disorder means regular hospital visits are now part of his life.
“At the given time without a doubt I will use VAD, but not currently,” he said.
“I have grandchildren and two beautiful sons and daughter-in-laws and a wonderful wife and so their support has been amazing through all of this.
“They fully support this journey, so today’s a huge day and a lot of weight off my shoulders and many, many other people who are not well.
“I don’t have to leave my home, I can be with my family and not only me, but every single person who has a terminal illness has this amazing avenue to go down.”
Watson isn’t the only South Australian who is contemplating accessing VAD.
The chair of the state’s VAD review board, Dr Melanie Turner, said eight people contacted SA Health yesterday asking about accessing the service.
SA Health estimates that about 50 to 60 people will start the VAD process each month, while about 11 people will die from VAD each month, based on modelling from Victoria and Western Australia.
Since the legislation passed in 2021, a taskforce led by former Australian Medical Association vice-president Dr Chris Moy has been figuring out how the laws would be implemented.
Here, Moy and InDaily explain how the Voluntary Assisted Dying Act 2021 will work.
Explainer: How SA’s voluntary assisted dying system will work
- What is VAD?
- Who can access VAD?
- If you want to access VAD and believe you are eligible, what should you do?
- Can you ask any doctor about accessing VAD?
- What happens during the assessment process?
- What happens after the assessments?
- How long will it take between making a request for VAD and getting the medication?
- How do you get the medication?
- Can you choose where you die?
- What is the care navigator service?
- How many doctors are trained to assist with VAD?
- Can you use telehealth to access VAD?
- How much will it cost to access VAD?
- How many people are expected to access VAD?
- Where is the best place to go to get more information about VAD?
What is VAD?
VAD allows eligible people to voluntarily access and self-administer, or in some cases have a doctor administer, a medication that will cause their death.
There are multiple safeguards set out in the legislation which ensure that only eligible people can access VAD, and to protect people from being coerced into it.
Those who do not want to receive VAD will still have access to palliative care services.
“In palliative care, the aim of treatment is to maintain the comfort and dignity of the patient and to give them whatever medication is required to reduce pain and control their symptoms,” Moy explains.
“For voluntary assisted dying, a doctor assists a patient in being able to end their life at the time that they choose.
“It (VAD) is another choice, but it’s not going to replace palliative care.”
Who can access VAD?
“The criteria for access is very clear and the person has to meet all of the eligibility criteria,” Moy says.
Those wanting to access VAD in South Australia must:
- Be aged over 18 years.
- Be an Australian citizen or permanent resident.
- Have lived in South Australia for at least 12 months when they make their first request.
- Have decision-making capacity.
- Be acting freely and without coercion.
- Have been diagnosed with a disease, illness or medical condition that is incurable, advanced and progressive, will cause death within six months (or 12 months if they have a neurodegenerative disease), and is causing suffering in a manner that they consider is intolerable.
People with dementia, mental illness or disability cannot access VAD unless they meet all of the eligibility criteria, including having an advanced disease likely to cause death and decision-making capacity.
If you want to access VAD and believe you are eligible, what should you do?
Moy says if someone wants to access VAD, they must first raise the subject with a doctor such as their GP, or a nurse.
He says it is important for people to understand that doctors and other health workers are legally prevented from being the first to raise VAD as an option with patients.
“The individual has to bring up the subject themselves and have to request it (VAD) unambiguously before a doctor can discuss this as an option with them,” he says.
“It’s really important that patients understand that, otherwise they might wonder why a doctor might not be bringing up the subject.
“This is a protection which was put in (the South Australian legislation) which is in line with the Victorian legislation, which is trying to cover off the potential that a patient might feel that a doctor could be coercing them into this.”
Can you ask any doctor about accessing VAD?
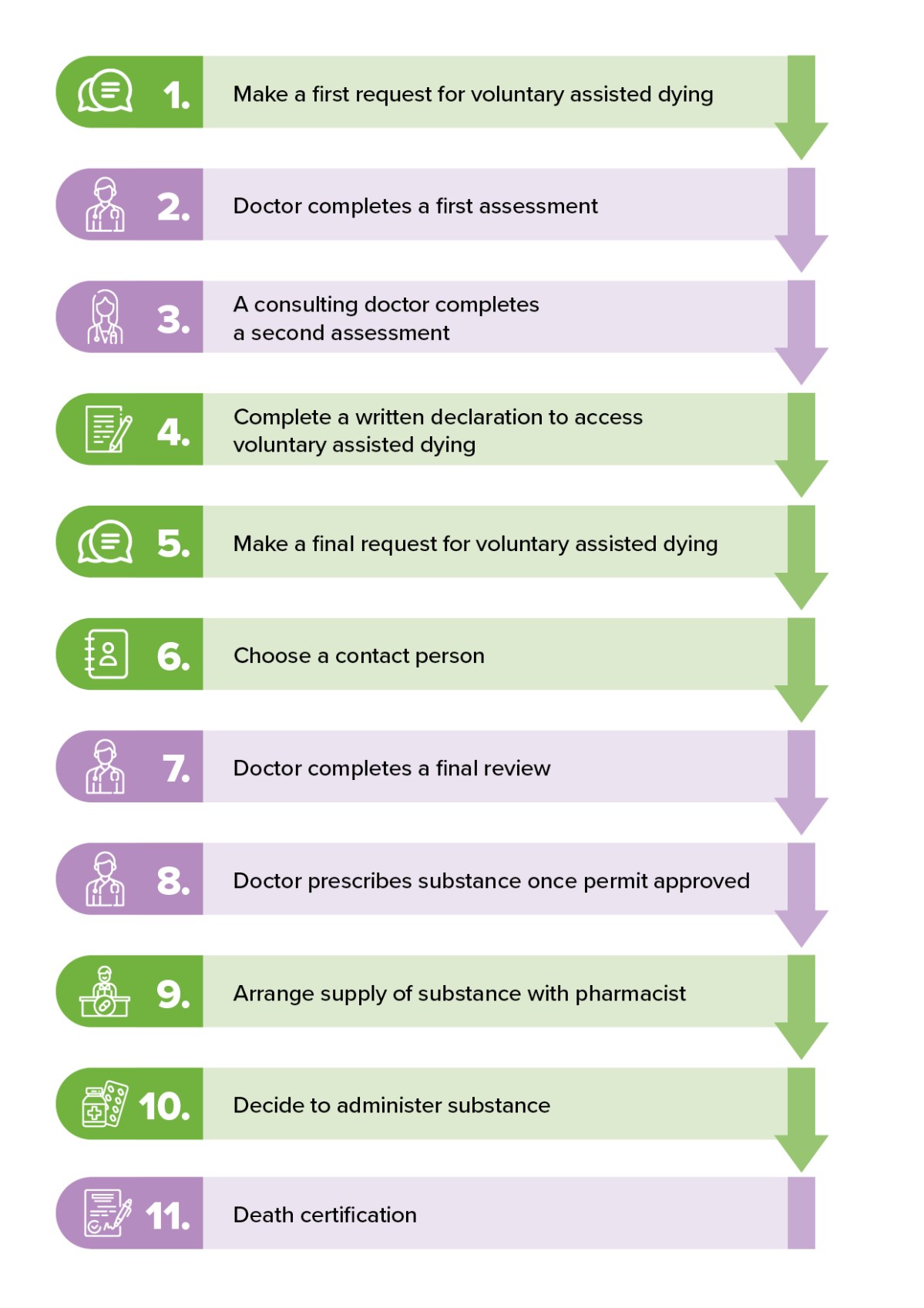
Image: SA Health
Patients can discuss VAD with any doctor, but not all will be willing or able to assist them.
Some doctors may conscientiously object to being involved, while others may not have undergone the required training to guide patients through the process.
“One would hope that most people have a good enough relationship with their GP to approach them and bring up the subject and ask them specifically,” Moy says.
“Hopefully, if the doctor is not able to assist, there will be backup options where the doctor will be able to assist that patient to find somebody who is able to provide the service.”
Moy says some doctors who aren’t trained to deliver VAD may be willing to do the training if a patient asks them. But he says the training can take a long time and not all of it is subsidised by Medicare.
SA Health has set up a “Care Navigator Service” (more details on that below), which can help link up patients to doctors who can help them access VAD.
Once a patient makes a first request for VAD, their doctor will do an assessment.
What happens during the assessment process?
“The assessment process is really a matter of first up, making sure the person is eligible,” Moy says.
“The doctor has to make sure that the patient is not being coerced and they also have to make sure the individual has decision-making capacity and they are doing this absolutely voluntarily.
“As part of that, they may need to refer the patient on to other specialists, for example, to make sure that person has decision-making capacity or that the prognosis is correct – that it is within six months or 12 months (of death).”
Once the doctor is satisfied that their patient is eligible, they will then refer them to a second doctor to do another assessment.
“Therefore, there is a minimum of two doctors going through to make sure that the patient fits all the criteria, isn’t being coerced, has decision-making capacity, is doing it voluntarily,” Moy says.
What happens after the assessments?
Once a patient is assessed by at least two doctors, they must complete a written declaration to access VAD.
The patient must then make a final request, after which the doctor will undertake a final review.
Only then can a doctor prescribe the medication and approve a permit.
How long will it take between making a request for VAD and getting the medication?
Moy says the legislation states that it must take a minimum of nine days between a patient requesting VAD and them being able to access it.
The length of time will depend on which doctors are involved and whether a patient requires additional specialist assessment.
How do you get the medication?
Most people accessing VAD will self-administer the medication that will cause their death.
Moy says once a doctor prescribes the medication, a special pharmacy service set up at the Repat Health Precinct at Daw Park will liaise with the patient to work out when they can obtain it.
“(The medication) will be contained in a locked box with only two keys – one key for the individual and one key held by the Voluntary Assisted Dying Pharmacy Service,” he says.
“The patient will be given the key directly and they can hold on to it as long as they like.
“At the time of their choosing, they can access the medication, mix it and take it.”
Doctors will only administer medication intravenously if a patient has trouble digesting.
“Having it done intravenously is a far more complex procedure and it’s far more limiting in terms of choice of when it is done,” Moy says.
Can you choose where you die?
“Absolutely,” Moy says. “The vast majority of individuals will choose to die in their home and that may include aged care facilities.”
Unlike in Victoria, Moy says aged care facilities in South Australia are prevented from impeding residents from accessing VAD, regardless of whether staff or the organisation conscientiously objects to the practice.
“The organisations don’t have to provide or support this, but they cannot impede the provision of any aspect, including the individual obtaining the medication and taking it at the time that they want,” he says.
“We’ve done a fair bit of work to support aged care facilities with this.”

Supporters of voluntary assisted dying during a candlelight rally on the steps of Parliament House. Photo: Kelly Barnes/AAP
What is the care navigator service?
“Care navigators” are nurses and allied health professionals with experience in complex and end-of-life care, who have been tasked with managing queries about VAD, connecting patients to doctors and facilitating connections between services.
A VAD liaison nurse has been appointed in each of the three adult metropolitan local health networks, with another nurse to be recruited for regional South Australia.
“Their job will be to first up provide information to both patients and health practitioners to be able to link up the right doctors who can provide the service to patients,” Moy says.
“They will also be able to make sure all steps are followed through and people are guided throughout the process as much as possible.”
How many doctors are trained to assist with VAD?
Moy says there are about 50 doctors who are registered and in the process of getting trained.
He says training will continue to be made available to doctors after January 31.
“What is likely to happen is doctors are going to be asked about this and they might look into it and do the training then if they’re comfortable,” he says.
“Although we’d like to have as many doctors trained on day one, we also understand that it’s important to build up momentum after the 31st of January.”
Can you use telehealth to access VAD?
According to Moy, the Commonwealth Criminal Code currently prevents doctors from using any carriage facility – including phone, teleconference or email – to discuss supporting patients to end their life.
He says the rule is a “major concern” because it could impede people’s access to VAD in regional areas.
“It acts as barrier, for example, if the specialist pharmacist needs to support a doctor who isn’t familiar with this to be able to prescribe the medications and for a patient to know what to do in terms of taking the medication,” he says.
“Until that’s changed, it’s actually complicating the provision of voluntary assisted dying in a state as large as ours.
“There’s a lot of support to make sure the pharmacist can actually travel into the country, or that patients can come into town to be able to get information directly.”

Photo: Bianca de Marchi/AAP
How much will it cost to access VAD?
The cost depends on a patient’s doctor.
“The medications are only through one pharmacy service – the SA Voluntary Assisted During Pharmacy Service – and they’re going to be subsidised, but provided at the same amount that people would pay for normal medications,” Moy says.
“In terms of the cost of the service, it will depend on a patient’s doctor and whether there is provision within SA Health.
“Medicare will cover some of the cost – like consultations and that sort of thing – but it’s worth talking to your doctor about it.”
How many people are expected to access VAD?
The VAD implementation taskforce estimates that about 50 to 60 people will start the VAD process each month, while about 11 people will die from VAD each month, based on modelling from Victoria and Western Australia.
Where is the best place to go to get more information about VAD?
SA Health has information on its website about accessing VAD.
Moy says printed information sheets and booklets will also be sent to general practices, councils, hospitals, MP offices and clinics.




