Double blow for SA’s mentally ill


Pat Sutton has struggled to have her son's physical health assessed for more than 20 years. Photo: Nat Rogers/InDaily
A punch thrown at 21-year-old Peter Sutton’s head injured his brain and shattered his jaw.
He fell to the ground, where he was repeatedly kicked in the head.
His friends took him away from the party, and back to his house. His head was swelling and he was covered in blood. They rushed him to hospital.
Peter’s attacker pleaded guilty to assault causing actual bodily harm, and received a suspended sentence.
Today, Peter is almost mute, and suffers from cognitive impairment, schizophrenia and anxiety, diabetes and rotting teeth.
He is 44 years old and is cared for by his parents, Pat and Keith.
His brother, Ben, was a straight-A student before he began to develop schizophrenia at the age of 17.
Pat and Keith also care for Ben in the family home.
“My husband’s 70 next year, and I’m only a few years behind him, and we’ve been looking after them now for 23 years,” Pat says.
“What’s going to happen to our sons when we’re no-longer able to support them?”
The repeated tragedies suffered by the Sutton family over past the 23 years have only been compounded, says Pat, by their experience of the South Australian health system.
“You have no idea how many failures we’ve had,” she says.
One of the most distressing of these, Pat says, has been a failure to have Peter’s physical health conditions assessed and treated.
The catch-22 for Peter is that, like many people who suffer schizophrenia, he is unable to recognise his physical or mental illnesses. This condition is called anosognosia.
No-one can force him to see a doctor or a dentist, and nothing his parents has tried has been able to establish the assertive, regular care he needs for his physical health conditions.
According to Pat, assessments of Peter’s physical health are rare. His conditions deteriorate, and he returns to hospital.
Currently, Peter has a suspected cancer on his forehead, which has gone untreated.
When Pat asked Peter’s psychiatrist – who makes house calls – to examine it, he told her it was not his job to do so.
“I asked if he could look at the cancer on his forehead, because he’s a doctor, obviously,” she says.
“And he said: that’s really the GP’s job.”
In a statement to InDaily, SA Branch Chair of the Royal Australian and New Zealand College of Psychiatrists (RAZCP) Dr Michelle Atchison said the organisation “places an emphasis on their trainees understanding the need to be current with their medical knowledge and to be able to perform targeted and appropriate physical examinations”.
Pat continues to make appointments for her son’s potential cancer to be assessed at the Queen Elizabeth Hospital, but Peter refuses to go.
When Pat complained about a separate incident involving Peter’s discharge from the Queen Elizabeth Hospital in 2006, a letter from the Mental Health Division of Port Adelaide Community Treatment Team said her expectations of the team were “at odds with what we consider to be our functions and service philosophies (to be)”.
“… We monitor aspects of a client’s physical health and are proactive in this regard to clients who are on medications which may contribute to metabolic disorders. However we neither diagnose nor treat these conditions, this being the province of the GP in the first instance.”
Fortunately, Peter now has access to a service which video-calls him twice a day to make sure he takes the insulin which keeps him alive, run by the Royal District Nursing Service.
“That’s the only thing that works with my son,” Pat says.
Last week, Pat received news that the family’s struggle to get regular physical health assessments for Peter over more than two decades might be over.
An intermediate care centre is considering making an extraordinary arrangement which would see Peter taken to receive physical health assessments there, once every three months.
But for many South Australian families, the struggle continues.
InDaily has obtained an SA Health report which shows that nine out of 10 South Australians in the community mental health system did not receive a physical health assessment in the second half of last year.
The Mental Health Act states that: “there should be regular medical examination of every patient’s mental and physical health”.
SA Health would not say what it understands to be the definition of “regular” in the Act.
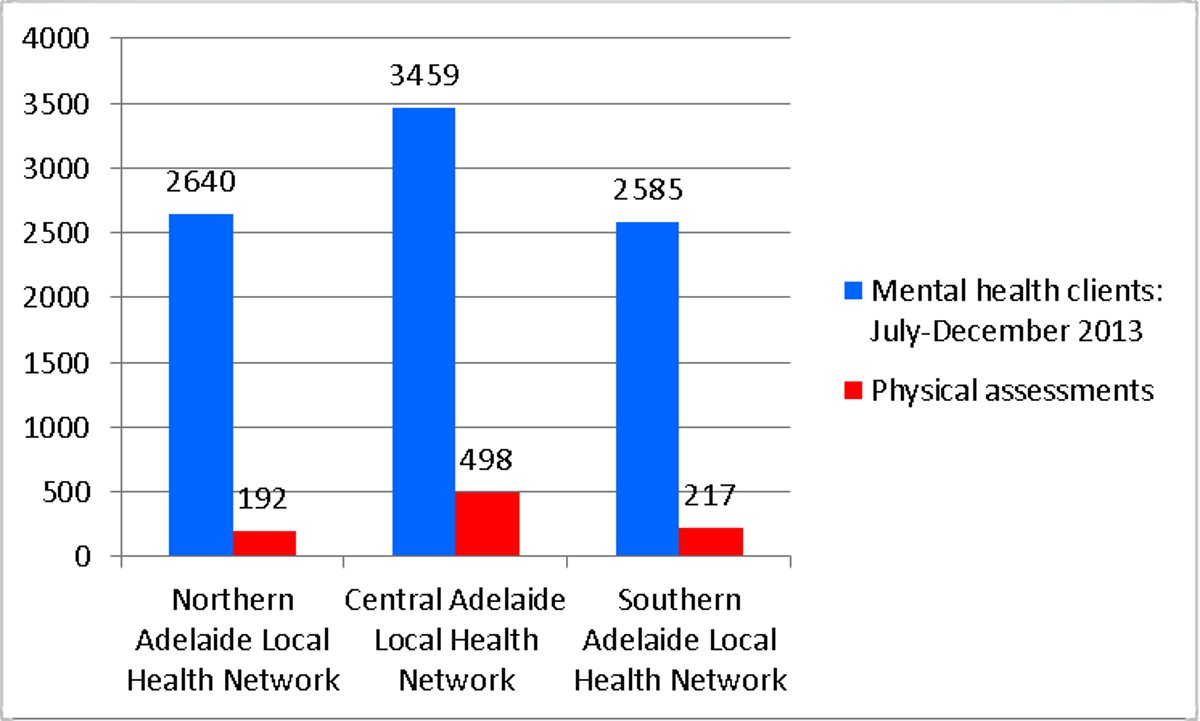
The number of mental health clients seen in the second half of 2013 and the number of physical assessments conducted, excluding emergency department, consultation liaison, private and triage.
The Mental Health Coalition of South Australia (MHCSA) wants a comprehensive physical health strategy to be established for people with severe, long-term mental illness.
“No-one in mental health thinks that we have done enough to address the physical health needs of people with mental illness,” says MHCSA Executive Director Geoff Harris.
“… but there has been increased awareness of the problem and some improvements in how we deliver services.
“Increasing the lifespan of people with mental illness should be a clear target of the Australian and South Australian mental health systems and there should be regular reporting on progress.
“The emphasis on physical health checks is an important part of the solution but we need to ensure that we are actually getting results.”
People who suffer mental illness in Australia are likely to die between 10 and 32 years younger than other Australians.
According to the Public Advocate, Dr John Brayley, “physical health assessment, and then advice and intervention, is essential in reducing this gap in both physical illness and mortality”.
“This is a widespread, significant issue. It is a national issue and we need better reporting across the country so that we can compare the performance of mental health systems in different states,” he says.
“It is difficult to say whether (a lack of physical health assessments) is the main cause (of the gap in life expectancy), but it’s a fundamental part of the response.”
SA Health issued a statement to InDaily citing data from June this year.
It shows that 96 per cent of consumers who had a high physical health risk, due to their prescribed medication, received physical health assessments when attending community mental health services.
“All mental health consumers are encouraged to receive regular physical health assessments,” the statement reads.
“These assessments are generally undertaken by a consumer’s treating GP and these checks are not captured in this report.
“SA Health works closely with the independent GPs to ensure our consumers receive appropriate physical and mental health care at all times.”




